Start the conversation with LUCEMYRA®
LUCEMYRA is the only FDA-approved, non-controlled treatment for the relief of multiple symptoms of opioid withdrawal in adults1

Photos within this website are actor portrayals.
LUCEMYRA is an in-patient or out-patient treatment for patients experiencing:

Opioid Detox
Help patients mitigate withdrawal symptoms when seeking an opioid-free in-patient or out-patient treatment program.
Initiation of Buprenorphine
Prior to the induction of sublingual buprenorphine, ease patients through the 72-hour period of abstinence often needed to avoid precipitating withdrawal.
Transition from Methadone
Help alleviate withdrawal symptoms in patients discontinuing methadone prior to a buprenorphine regimen.
Transition to Extended-Release Naltrexone
Help mitigate withdrawal symptoms during the 7- to 14-day abstinence period for patients transitioning to extended-release naltrexone injections.
Unplanned Disruptions in Treatment
Help mitigate withdrawal symptoms in patients with unplanned disruption of opioid treatment when opioid-agonists are unavailable or inappropriate for the situation.
After-Treatment Care
Help patients who have completed a successful MAT regimen with buprenorphine or methadone and are set to experience withdrawal symptoms from final step-down off treatment.
Opioid Detox
Help patients mitigate withdrawal symptoms when seeking an opioid-free in-patient or out-patient treatment program.
Initiation of Buprenorphine
Prior to the induction of sublingual buprenorphine, ease patients through the 72-hour period of abstinence often needed to avoid precipitating withdrawal.
Transition from Methadone to Buprenorphine
Help alleviate withdrawal symptoms in patients discontinuing methadone prior to a buprenorphine regimen.
Transition to Extended-Release Naltrexone
Help mitigate withdrawal symptoms during the 7- to 14-day abstinence period for patients transitioning to extended-release naltrexone injections.
Unplanned Disruptions in Treatment
Help mitigate withdrawal symptoms in patients with unplanned disruption of opioid treatment when opioid-agonists are unavailable or inappropriate for the situation.
After-Treatment Care
Help patients who have completed a successful MAT regimen with buprenorphine or methadone and are set to experience withdrawal symptoms from final step-down off treatment.
Discover how LUCEMYRA helped patients relieve the symptoms of opioid withdrawal
Play Video
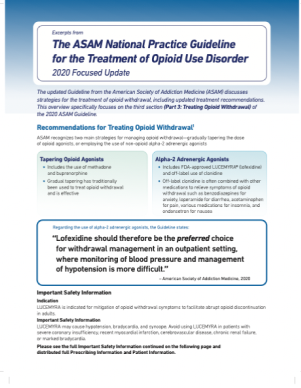
2020 ASAM National Practice Guideline: Recommendations for Treating Opioid Withdrawal2
The American Society of Addiction Medicine (ASAM) recognizes two main strategies for managing opioid withdrawal: gradually tapering the dose of the current opioid(s), or using a non-opioid medication, like LUCEMYRA (lofexidine).
Regarding the use of alpha-2 adrenergic agonists, the Guideline states:
“Lofexidine should therefore be the preferred choice for withdrawal management in an outpatient setting, where monitoring of blood pressure and management of hypotension is more difficult.”
-American Society of Addiction Medicine, 2020
Learn more about the 2020 ASAM Guidelines
- LUCEMYRA® (lofexidine) [Prescribing Information]. USWM, LLC; 2020
- Data on file. US WorldMeds; 2017. 7. (ASAM). National practice guideline for the treatment of opioid use disorder: 2020 focused update. 2020. https://www.asam.org/Quality-Science/quality/2020 -national-practice-guideline. Accessed July 13, 2020.



